What is Veal Chop Nursing? Veal Chop Mine mnemonic is an acronym that relates to electronic fetal monitoring. It is a quick way to remember fetal heart rate decelerations and what they are caused by. Veal is the type of heart deceleration, the Chop is the cause of the deceleration, and mine are the interventions needed for the deceleration. Read below for a further description of Veal Chop Nursing.
What you will learn in this article:
What is Veal Chop Nursing?
WHat are the Veal Chop decelerations?
What are the Veal Chop Interventions?
Veal Chop Mnemonic
The veal chop nursing acronym is a great way to help you remember fetal well-being, but the goal is to help you remember without it.
Variables are caused by Cord Compression
Early decels are caused by Head Compression
Accelerations indicate an Okay Oxygenated Baby
Late decels are caused by Placental Insufficiency
Veal Chop Mine Nursing
Veal Chop Mine is a mnemonic for learning the basics of fetal heart decelerations, their cause, and how to fix them.
The VEAL portion of the VEAL CHOP acronym has to do with the type of deceleration or acceleration:
V – Variable Decelerations: These abrupt decelerations in fetal heart rate are often caused by Cord Compression, where the umbilical cord experiences pressure, affecting oxygen and nutrient supply to the baby.
E – Early Decelerations: These gradual heart rate decreases are typically caused by Head Compression, a natural physiological response to fetal head compression during uterine contractions.
A – Accelerations: These are abrupt increases in the fetal heart rate that signify fetal well-being and are not associated with any particular cause. These just indicate good fetal oxygenation.
L – Late Decelerations: This delayed fetal heart rate decrease usually results from Uteroplacental Insufficiency, where there is compromised oxygen and nutrient exchange between the placenta and the fetus.
The CHOP component of the VEAL CHOP mnemonic further delves into specific deceleration causes:
C – Cord Compression (Variable Decelerations): Cord compression can stem from factors such as the umbilical cord being compressed between the fetus and the maternal pelvis or being looped around the fetus. Typically the umbilical vein and umbilical arteries become compressed, which causes abrupt fetal bradycardia (low fetal heartbeat).
H – Head Compression (Early Decelerations): Head compression occurs during contractions, leading to a temporary reduction in blood flow to the fetus's head.
O – Okay (Accelerations): Well-oxygenated baby with moderate variability and accelerations present.
P – Placental Insufficiency (Late Decelerations): Poor placental perfusion compromises the exchange of oxygen and nutrients between the mother and fetus, leading to late decelerations. These decelerations indicate fetal distress and fetal hypoxia.
The MINE portion of the VEAL CHOP mnemonic refers to specific interventions for fetal heart decelerations:
M - Move the mom and change positions: Turning to a different side or hands and knees can help resolve variable decelerations if the baby is lying on its cord.
I - Interventions not needed: With early decelerations, the head squeeze and drop in fetal heart rate are normal. Do nothing.
N - No intervention: Interventions are not necessary for moderate variability and accelerations. This means that the baby is doing well with oxygenation and nutrients.
E - Evaluate: Evaluate why the mother could be having late decelerations. Remember that this means there is some form of transient ischemia and that there is insufficient blood flow between the placenta and the baby. Interventions include fluid, position change, turning off pitocin, turning down pitocin, and increasing blood pressure or oxygen as a last resort (if the 02 is not within normal limits).
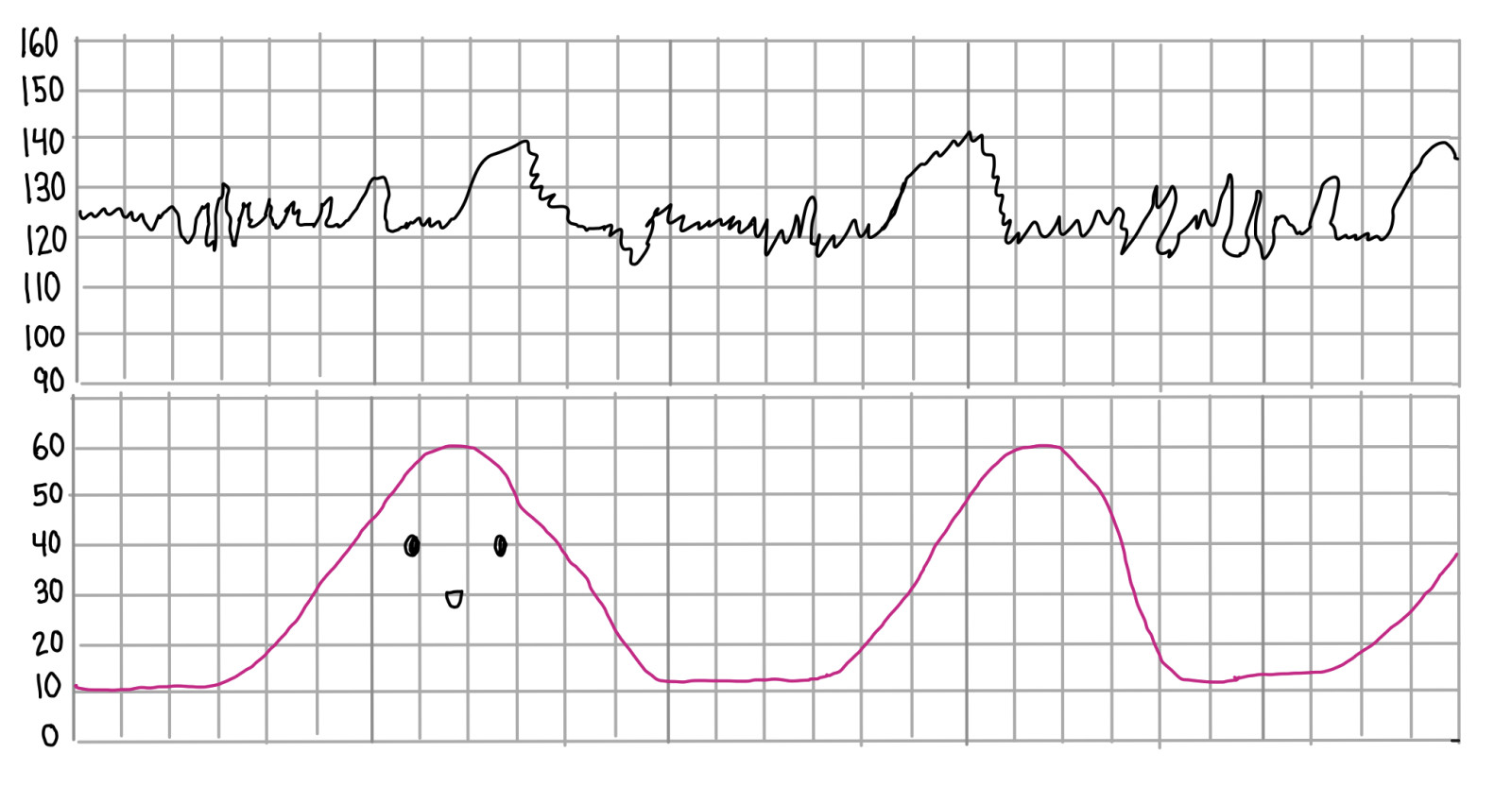
Veal Chop Fetal Monitoring
There are different types of fetal heart rate decelerations that are both abnormal and normal given the physiological changes that occur in labor. The different types of decelerations include late decelerations, variable decelerations, early decelerations, and prolonged decelerations. We can take a look at veal chop nursing strips.
Veal Chop Decelerations:
Variable Decelerations
A variable deceleration is a decrease in the heart rate that is faster to the peak (nadir) and tends to be shaped like a V. Variable decelerations are caused by the umbilical cord being compressed inside of the uterus. Cord compression could be with or without a contraction. The cause of the quick drop in the fetal heart rate is the quick and aggressive blood supply cut off from the umbilical cord being squished. Smaller variables are physiologically normal in early gestation and can be due to fetal movement, but as they become term, variables are typically more due to a loss of amniotic fluid or low amniotic fluid.
Interventions: Variables can be resolved usually by position changes, oxytocin reduction or discontinuation, or amnioinfusions. Amnioinfusions use normal saline infused into an intrauterine pressure catheter (IUPC) to give fluid back into the uterus. The strip is considered a category 2 strip if it has variables present.
For more advanced information if you are interested in being an L&D nurse:
Variable decelerations have to be at least 15 seconds wide in total, and 15 seconds deep in the variable deceleration, with the lowest point or nadir of the decelerations being shorter than 30 seconds. If it takes longer than 30 seconds to get to the lowest point, it may be a different deceleration based on the location and what it looks like.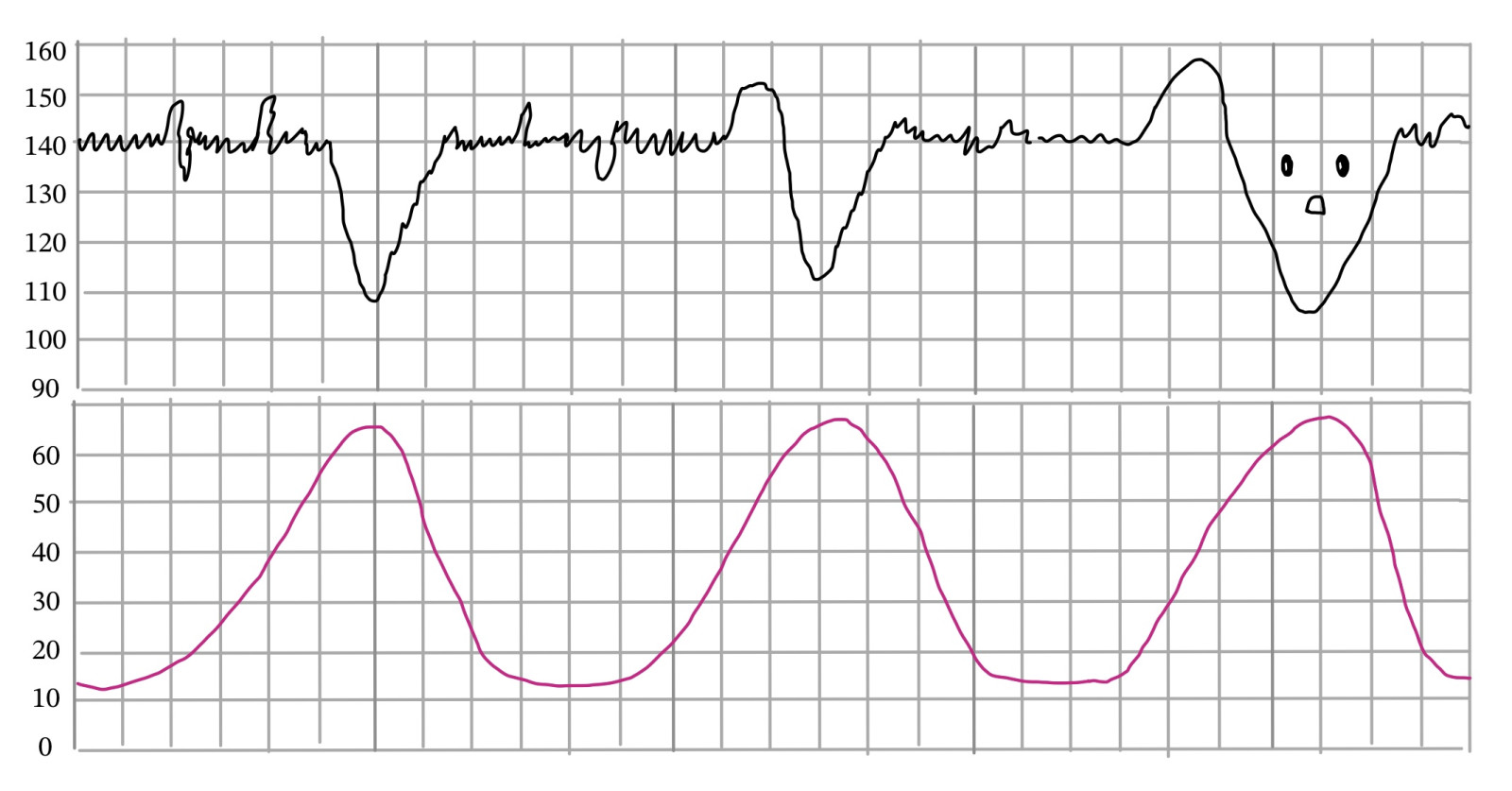
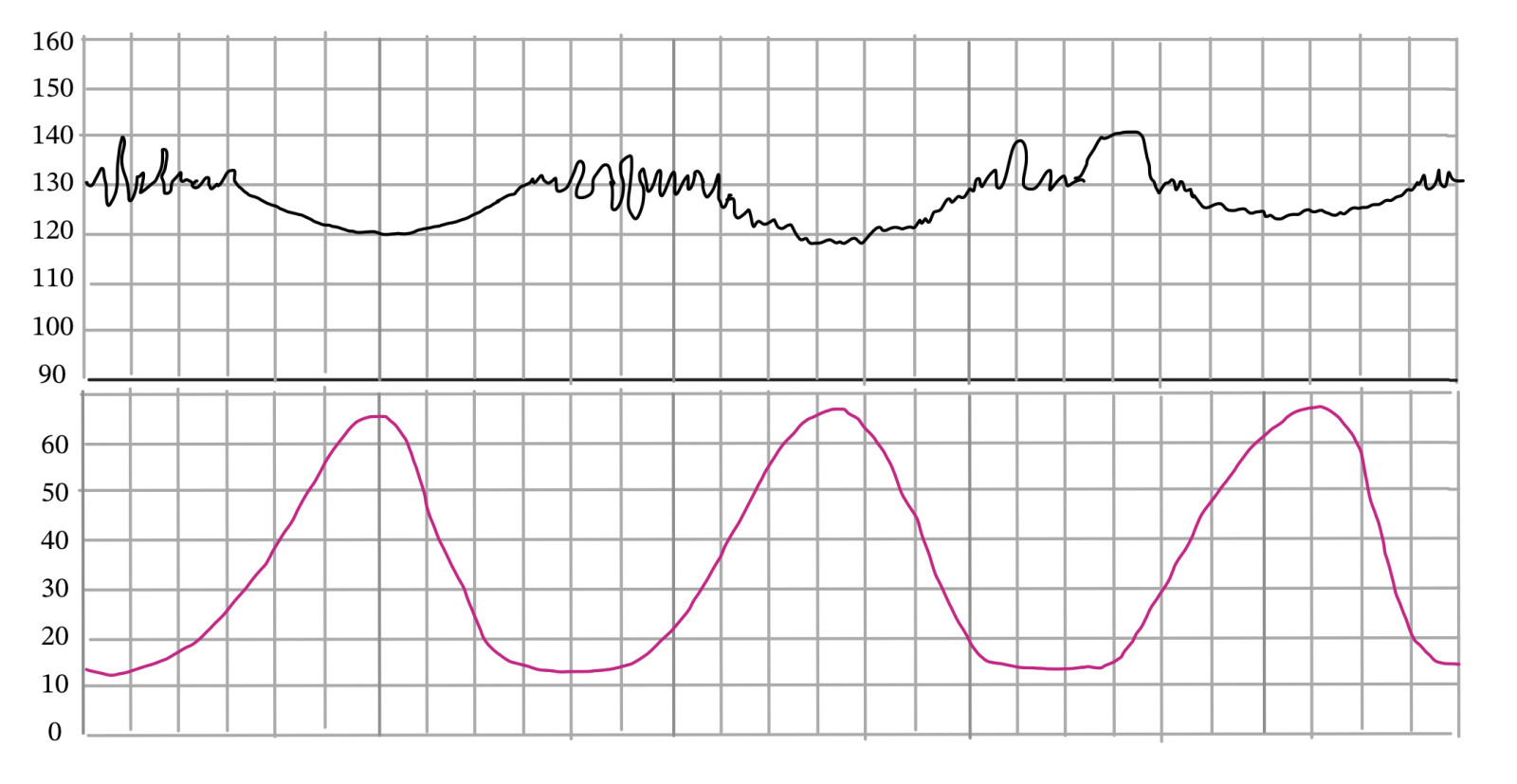
Early Decelerations
Early decelerations are decelerations that mirror contractions. The most important portion when differentiating late versus early decelerations is that the peak (or nadir) must match the nadir of the contractions. Early decelerations are a normal physiological process and indicate that the head is being compressed within the pelvis from the contraction. The drop in the fetal heart rate is due to the vagus nerve being stimulated, which decreases the heart rate. When pushing, you will usually see a decrease in the fetal heart rate with the pushing, due to the vagal stimulation. Which is a normal physiological effect.
Interventions: Continue to monitor or cervical exam if feeling pressure.
For more advanced information if you are interested in being an L&D nurse:
An early deceleration has a slow descent to the nadir from baseline. It is a slow gradual drop to the nadir being at least 30 seconds from the baseline to the peak of the deceleration. A strip is considered a category 1 strip if it has early decelerations present because they are considered normal.
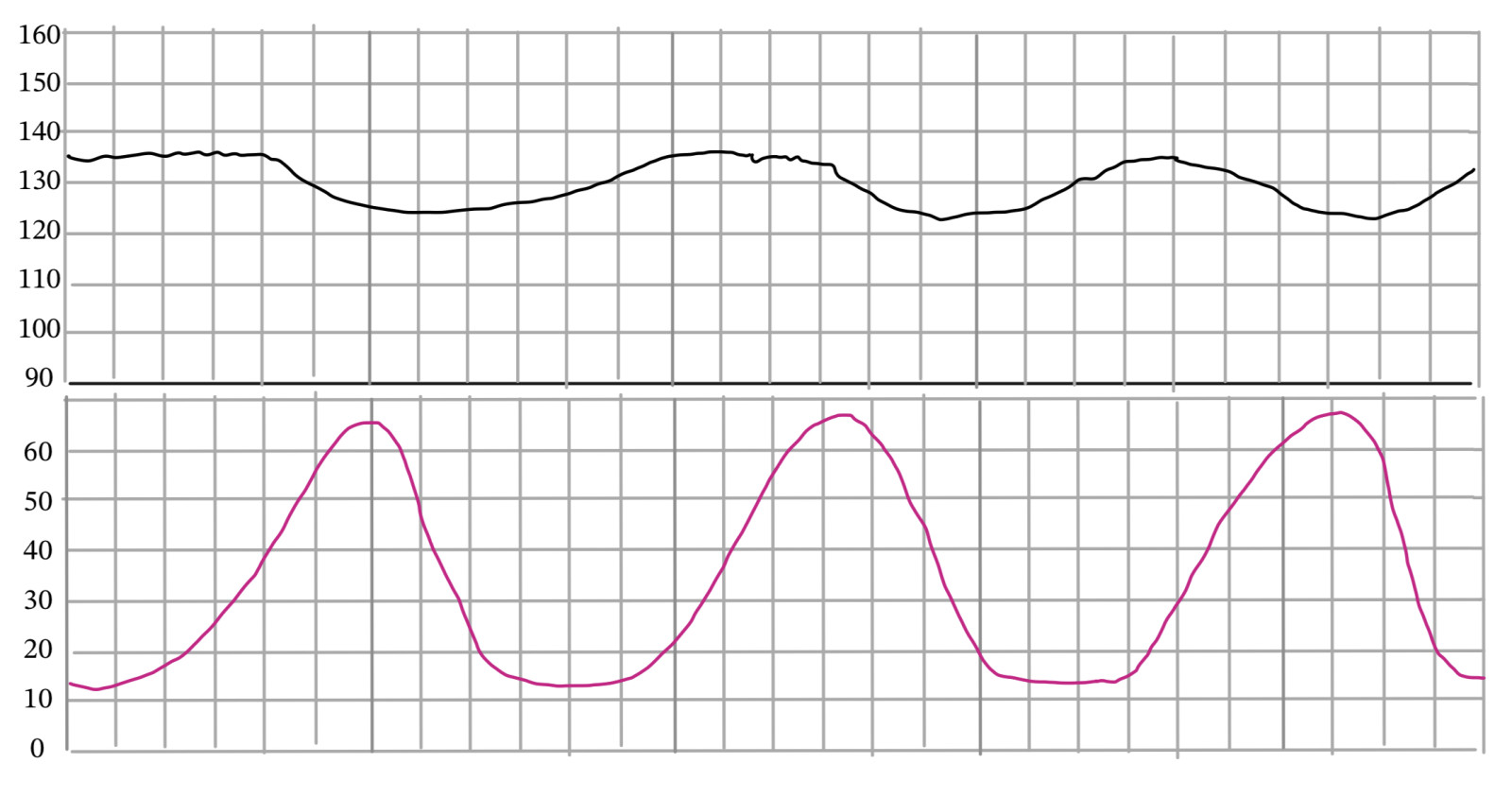
Late Decelerations
Late decelerations are decreases in the fetal heart rate where the peak or the nadir of the deceleration is after the contraction. Late decelerations are "late" and present after the contractions. Late decelerations indicate that there is placental insufficiency or transient ischemia to the baby. This can be due to maternal hypotension from an epidural (which is a temporary ischemia that can be resolved with fluids and medications). Lates can be present with moderate variability, but if the ischemia maintains and is still present, the moderate variability turns into minimal variability. If the minimal variability and lates persist it will lead to fetal acidemia.
Interventions: Late decelerations can be resolved usually with position changes, oxytocin reduction or discontinuation, and additional fluids. Late decelerations require intrauterine resuscitation to increase oxygenation back to the fetus. The strip is considered a category 2 strip if it has a late deceleration present.
For more advanced information if you are interested in being an L&D nurse:
Late decelerations are a slow descent to the peak or nadir, with the peak of the deceleration being after the nadir of their contraction. The descent must be at least 30 seconds to the nadir of the deceleration. Late decelerations descend, peak, and recover after a contraction typically. Some late decelerations recover at the same time as a contraction, but the nadir will still be after the nadir of the contractions. It's all about the nadir!
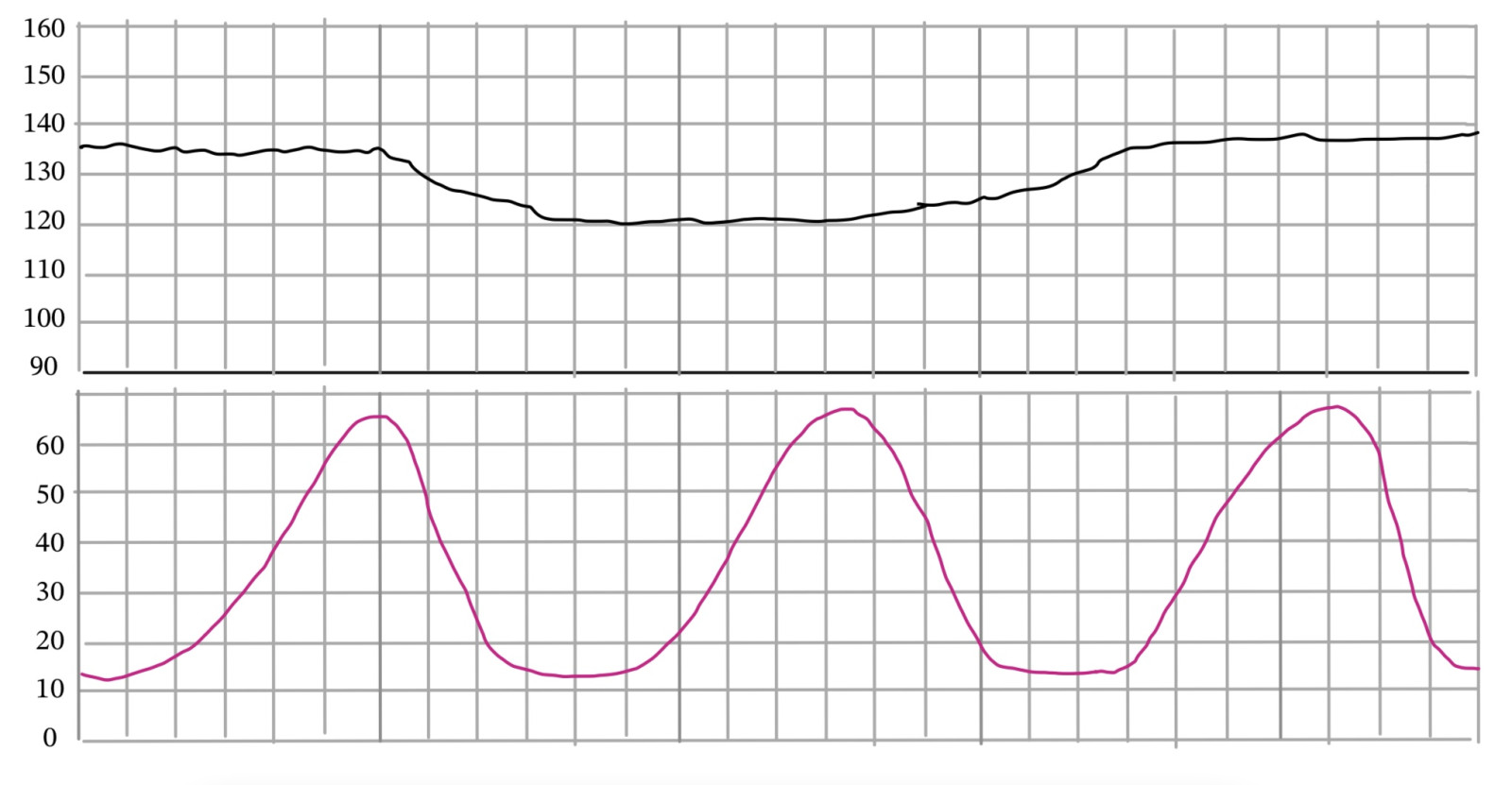
Prolonged Decelerations
Prolonged Decelerations are a decrease within the fetal heart rate being at least 15 seconds deep and lasting at least two minutes long but not more than 10 minutes. You must intervene with prolonged decelerations immediately because the baby is not getting the blood flow it needs and is stressed. The fetal cardiovascular system relies on a steady supply of blood, which carries oxygen and nutrients, to support growth and development. A prolonged deceleration, in essence, represents a moment where this vital nourishment is compromised.
Interventions: Prolonged Decelerations can be resolved sometimes with fluids, position changes, oxytocin discontinuation, and oxygen. Terbutaline can be given to stop contractions to allow the baby to recover.
The strip is considered a category 2 strip if it has a prolonged deceleration present.
Accelerations and Variability
The best indicator for a well-oxygenated baby is a good moderate variability. Accelerations are additional indicators that a baby is well-oxygenated and is responding to stimuli with heart rate increases. Fetal tachycardia is different from an acceleration and does not indicate fetal well-being. Category 1 strips have moderate variability and can have accelerations. It is not a requirement for a fetal strip to have accelerations to be a category 1 strip. However, in order to be a reactive NST, which is different from a category 1 strip, they must have at least two accelerations within 20 minutes.
Accelerations indicate a happy, well-oxygenated baby.
Remember: NST's are 20-minute fetal heart rate monitoring tests done to check on the well-being of a fetus. A reactive NST means the baby had 2 accelerations within 20 minutes, and a nonreactive NST means they did not have 2 accelerations within 20 minutes.
For more advanced information if you are interested in being an L&D nurse:
Accelerations must be 15 seconds high and 15 seconds long for it to be considered an acceleration for a baby over 32 weeks gestation. A baby under 32 weeks may have accelerations that are 10 seconds high and 10 seconds long. However, if a baby that is 31 weeks has a 15 by 15 acceleration, a 10 by 10 acceleration is no longer the standard. This is because it means the baby's neurological system has developed well enough that it can now have 15 by 15 accelerations in response to stimuli.
Additionally, if you have minimal variability, you could question if a fetus is starting to have academia, but if the minimal variability can still produce an acceleration from head stimulation, it is still reassuring that the fetus is okay.
Veal Chop Nursing Interventions
1. Change Maternal Position: Sometimes, changing the mother's position can help alleviate pressure on the umbilical cord or improve blood flow to the placenta, which can impact the fetal heart rate. For example, if the mother is lying on her back, changing to a lateral position might be beneficial.
2. Administer Oxygen: Providing supplemental oxygen to the mother can help increase the oxygen supply to the baby, potentially improving fetal heart rate patterns.
3. Adjust Maternal Fluids: Intravenous fluids might be adjusted to help optimize blood flow to the placenta and the baby.
4. Discontinue Oxytocin (Pitocin) Infusion: If the mother is receiving oxytocin (Pitocin) to induce or augment labor, stopping or reducing the infusion might be considered to reduce stress on the baby.
5. Amnioinfusion: In cases of variable decelerations caused by cord compression, amnioinfusion involves infusing sterile saline into the uterus to cushion the umbilical cord and reduce compression effects during contractions.
6. Maternal Position Changes: Changing the mother's position, such as moving from supine to lateral or hands-and-knees, can alleviate pressure on the vena cava and improve fetal heart blood flow.
7. Adjusting Uterine Activity: If contractions are too frequent or intense, medications like tocolytics might be used to temporarily reduce uterine activity, giving the fetal heart rate a chance to recover.
8. Provide Fluids and Medications to Mother: Intravenous fluids can help improve maternal blood pressure and perfusion to the placenta, while medications like terbutaline can relax the uterus and potentially alleviate decelerations.
9. Fetal Scalp Stimulation: Gentle stimulation of the baby's scalp during a vaginal exam can sometimes provoke a reaction that improves the fetal heart rate pattern.
10. Internal Fetal Monitoring: If external monitoring isn't providing a clear picture of the baby's well-being, internal monitoring via a fetal scalp electrode can provide more accurate data on the fetal heart rate.
11. Expedite Delivery: In cases of severe or persistent decelerations, if the situation warrants it, healthcare providers might recommend expediting delivery through methods like cesarean section.
It's important to note that the choice of intervention will depend on the clinical judgment of the healthcare provider, the specific circumstances of the labor, and the condition of both the mother and the baby. The goal is to ensure the safety and well-being of both individuals while closely monitoring the fetal heart rate patterns and making timely decisions based on the information available.
Veal Chop Mine Nursing
Veal Chop OB mnemonic is a great way to remember important fetal heart decelerations and accelerations. Electronic fetal monitoring is a helpful way for nurses and doctors to monitor fetal well-being. Remember that variables are for cord compression, which is why you get the fast aggressive drop that is in the shape of a V. Early decelerations are for head compression, and are completely normal decelerations present when the vagus nerve is being stimulated and the head is coming down into the pelvis. Accelerations mean the baby is happy and well-oxygenated. Lates mean there is placental insufficiency and that ischemia is present. Think about the process of blood flow and oxygenation when trying to remember what type of fetal heart decelerations happen with specific events. Remember when studying for the NCLEX you should know these decelerations and their interventions. Understanding fetal heart rate monitoring is vital for understanding what is happening to a baby. I hope you enjoyed this article Veal Chop Nursing labor and delivery article.





